Summer can be a lively, carefree season for many. However, for individuals diagnosed with diabetes, it is important to put forth extra effort to properly manage blood glucose levels in the warmer months.
Studies have shown that patients with diabetes visit the emergency room and are hospitalized in greater numbers during warm-weather seasons as well as during heat waves. This is partly due to the fact that individuals with diabetes may have an impaired ability to sweat due to nerve damage. When the body is not able to sweat, it is unable to effectively regulate body temperature, which may predispose individuals to heat-related illness.
For this reason, it is important to practice good habits when managing diabetes in warm weather. Below are a few things to keep in mind for the summer months:
Familiarize Yourself with the Signs of Heat-Related Illness
The Centers for Disease Control and Prevention defines the symptoms of heat exhaustion as:
- Heavy sweating
- Fast, weak pulse
- Cold, pale, and clammy skin
- Fainting
- Nausea or vomiting
- Weakness
And the symptoms of heat stroke as:
- Rapid, strong pulse
- Red, hot, dry or moist skin
- Body temperature of more than 103°F
- Possible unconsciousness
Tip: If practicing an exercise routine, exercise in an air-conditioned environment if possible, or early in the morning or at night when temperatures are not as extreme.
Manage Diabetes By Avoiding Sun Exposure
Avoiding sunburn can be extremely beneficial when managing blood sugar levels. According to the American Diabetes Association, long or short-term pain, such as that from sunburns, causes the body to release hormones that increase blood glucose levels.
If you go out into the sun, apply sunscreen, use sunglasses, and wear a hat. Wearing loose-fitting, light-colored, protective clothing may also help you stay cool and avoid excessive sun exposure.
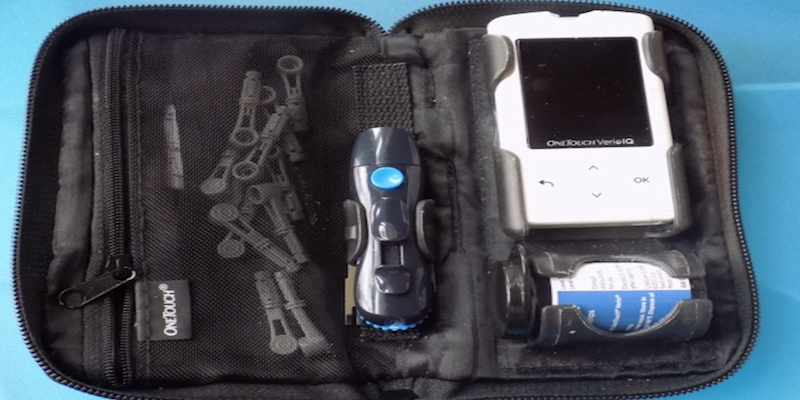
Protect Testing and Insulin Supplies From the Sun
Keep your insulin pump and testing supplies out of direct sunlight. Even in the shade heat can damage insulin and diabetes medical equipment. Familiarize yourself with safe storage temperatures and procedures included with the medical device and supplies packaging and adhere to these instructions.
Regularly Monitor Blood Glucose Levels
According to the Joslin Diabetes Center, individuals with diabetes should check their blood glucose levels at least 4 times a day when the weather is warmer, since heat can have a dramatic impact on blood glucose levels.
If you begin to experience any of the symptoms of heat exhaustion or heat stroke, you should check these numbers more often. Using a touchscreen insulin pump in conjunction with a Continuous Glucose Monitoring (CGM) device may help make glucose monitoring more convenient when there is a need for more frequent monitoring.
Monitor Fluid Intake
It is important to drink fluids even before feeling thirsty. Consult with your healthcare provider and diabetes management team on hydration during times of high heat if there are limitations set on your fluid intake.
Additionally, when blood glucose levels are high, this may trigger the body to excrete more urine, leading to rapid dehydration. For this reason, maintaining blood glucose levels will help keep the body hydrated.
Manage Diabetes With These Best Practices
Speak with your healthcare provider and diabetes management team for more information on how to best manage diabetes during the warm weather months. These individuals will be able to best help you prepare to fully enjoy the summer.
Resources:
http://www.mayoclinic.org/diseases-conditions/diabetes/expert-blog/heat-and-diabetes/bgp-20056563
http://www.joslin.org/info/Diabetes_Friendly_Tips_for_Handling_the_Summer_Heat.html
http://www.cdc.gov/features/diabetesheattravel/
https://www.endocrine.org/news-room/press-release-archives/2010/peoplewithdiabetesdonotknow
http://www.mayoclinic.org/diseases-conditions/anhidrosis/basics/definition/con-20033498
http://www.sweathelp.org/where-do-you-sweat/other-sweating/anhidrosis-no-sweating.html